“There were others!”
I thought as I cried tears of relief while reading the stories of two other mothers who had similar postpartum symptoms to the ones I was dealing with. Before that moment, I had no idea perinatal mood and anxiety disorders (PMADs) even existed, let alone what they looked like. So, there was zero chance that I would have been able to recognize the multiple warning signs (as obvious as they may have been) within myself.
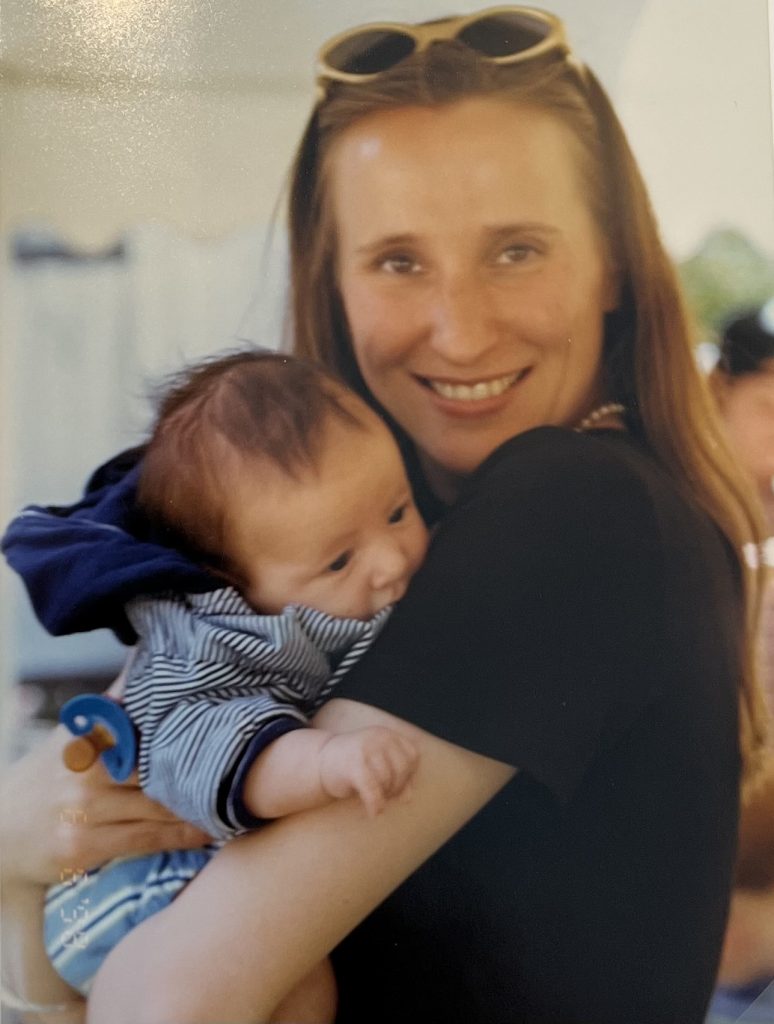
This was 25 years ago – I was completely unaware not only because I had never experienced the inner world of someone with mental illness, but also because it was 1998. Back then, there was a total lack of postpartum health education, and even had there been some, the internet was hardly available to the public, so quick and easy access to information was very limited.
There I was, 27 years old – deep in the trenches of postpartum depression and anxiety, and also dealing with an undiagnosed (and misunderstood!) case of postpartum OCD – terrified that I had turned into a crazy psychopath, and wondering if my baby and I could even coexist on this planet. And though my husband and I had (and still have) wonderfully supportive families, we were living alone in Berlin, Germany, as expats at the time, so reaching out for support was complicated, with my husband’s family being settled on the East Coast of the US and my family residing in Belgium.
My journey of healing and recovery ended up being long and hard. But in the end, it led me to finding a career I am passionate about to this day – a career as a therapist working with other parents coping with PMADs. It also led me to being bold enough to have another child 6 years after the birth of my son T., a baby girl in 2004, through open adoption.
This is my story. I’m sharing it with you because it may stand as a “There were others!” for you too (or for someone else you may know who could benefit from my story somehow.)
Preparing for Baby


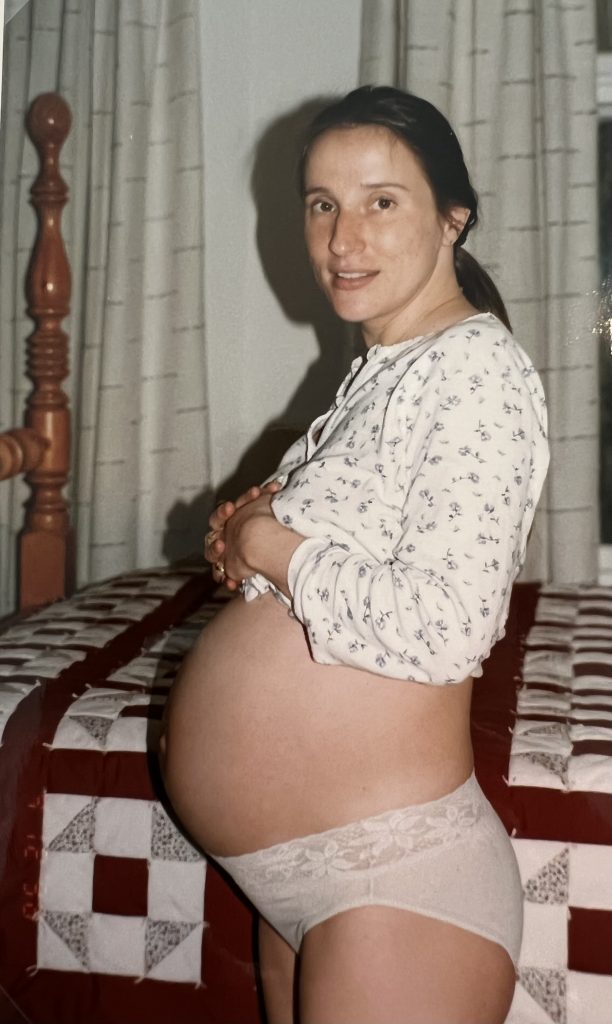
I always knew that I wanted to have children and that I wanted to be a relatively young mom, so my husband and I started trying three years after we were married.
After two failed pregnancies, one in the first trimester and one at the start of the second trimester, I was able to have a healthy pregnancy and carry baby T. full-term.
I loved being pregnant, every single moment of it, and ended up having a textbook pregnancy. I experienced some morning sickness during the first trimester, and then felt great the rest of the time. I also loved the “nesting” period and preparing for T.’s arrival. His due date was on my husband’s birthday, but he ended up being born four days early at 7 lbs. 9 oz. and 21 inches long.
The picture above to the left makes me laugh, the one with our 3 robes. I hung them up before T. arrived, and of course, his little, light blue robe ended up being purely decorative. The effort it took of putting that thing on him was never worth it. He wore it once, I took a snapshot, and that was the end of that.
In truth, I was one of those completely clueless, naive women before becoming a mother; I had absolutely no idea what I was getting myself into. Bringing a brand new, healthy baby, a “cute, little bundle of joy,” into this world (a time I had been dreaming of for many years), NOT being a time of sunshine and roses, came as a severe shock to my system.
Welcome to Motherhood

My welcome was not particularly warm. The German way did not provide the epidural when I wanted it. And on top of that, after eleven hours of the excruciating pain of labor and delivery, I started hemorrhaging because my uterine muscles would not contract. I learned later that this condition is called “atony of the uterus” and that, due to the risk of excessive amounts of blood loss, this can be life-threatening.
As soon as it became clear that my situation was uncontrollable, which was within minutes after T.’s birth, I was put under general anesthesia and hooked up to five different IV lines – two in both arms and one in my neck.
It took the work and expertise of eight doctors and nurses to save my life. I lost 3 liters of blood over 6 hours. Considering the average adult only has between 4.5 to 5.5 liters (and an extra 1.5 liters by the end of a pregnancy), I ended up losing approximately half my blood. Without the many blood transfusions I received, and the amazing medical care I was provided (minus the late epidural), I wouldn’t have had a chance of survival.
During those 6 hours, one of the nurses briefly left my room twice to tell my husband that they were doing everything in their power to stop the bleeding, but that they could not guarantee I was going to make it.
I spent two nights in the ICU and three more nights in a hospital room with two other new mothers and their newborns.
In the ICU, I barely slept because I was woken up by different machines that were attached to me doing their thing. There were a lot of loud beeping sounds and nurses constantly checking in on me day and night. And in the hospital room, between the three mothers with their three babies, at least one of us was always up with a baby, so it was impossible to sleep more than a few hours at a time then too.
So, after five nights of barely any sleep, I was so exhausted and so panicked about how depleted I felt, that I requested to go home. The nurses said that they would let me go if my blood counts were stable, which they were, so home I went.
“To the Depths of Despair”
That first night home from the hospital, I experienced my first panic attack ever. I did not know what it was back then, so I genuinely thought I was dying.
I told my husband to call 911. He called our doula instead, told her about my symptoms (mainly that I felt I was having an out-of-body experience), and she explained to him that it was anxiety I was experiencing. She suggested he help me settle down with some calming tea and meditation music. Neither helped much, so I ended up with another night, night #6, with no sleep. It was the next day that I started experiencing anticipatory anxiety, off and on throughout the entire day, about never being able to sleep again.
Feeling so anxious during the day about not sleeping at night, and then actually barely sleeping at night really started doing a number on me, as you can imagine, impacting my thoughts, my mood, and my health overall. This downward spiral I found myself in led me to start feeling very depressed, which in turn led me to stop nursing. No longer nursing added to my intense sadness.
Giving up nursing was one of the hardest decisions I ever had to make and one I regret making to this day, even though I know that under the same circumstances, I would make the same decision again considering I lost 30 lbs. in less than a month (due to no appetite and GI issues caused by anxiety). I clearly could not even nourish myself, let alone my infant.
Once I switched to bottle feeding, my spouse did all the nights even though I was wide awake for every single one of them. I thought selfishly that maybe if he was up more too, I had a better chance of surviving. He could then empathize with my exhaustion more. That thought didn’t necessarily make sense, and the amount of guilt I felt for even having these types of thoughts felt intolerable at times.
I should let my husband sleep if I’m up anyways; he has to be at work all day tomorrow. I’m a stay-at-home mom now. Isn’t that everything I ever wanted: a healthy baby and being able to stay home with him? How can I be so ungrateful? I must be spoiled rotten. All I have to do is take care of a newborn. If I can’t even do that, including giving night feedings, there has to be something seriously wrong with me. I’m clearly not cut out to be a mom.
And it wasn’t just the nights that were the problem.
My husband went back to work less than a week after I returned from the hospital, so I was really alone during those days. And motherhood did not come naturally to me. There was no “instant bond” or “baby bliss.” Being a mother felt strange to me, awkward even. I questioned myself about everything.
Do I put a blanket on him or not put a blanket on him? How about 2 blankets? Do I hold him or not hold him? Why would I hold him if he’s sleeping? Do I talk to him or not talk to him? Why would I talk to him if he can’t understand me nor reply? And the times when I do talk to him, why do I repeat myself and say everything twice? That’s just plain weird.
I literally questioned myself about everything. Am I supposed to play with him? But he’s so little, it doesn’t seem like he can really play yet. So, if I’m not sure whether I should hold him or not, or play with him or not, what am I supposed to be doing?
Oh, and what type of water should I put in his bottles?
I truly believed that if I put too much baby formula in his water or used the “wrong” type of water (for example, tap water as opposed to bottled water, or one brand of bottled water compared to another brand), it could kill him. Everything seemed dangerous, EVERYTHING. I felt like I was going crazy.
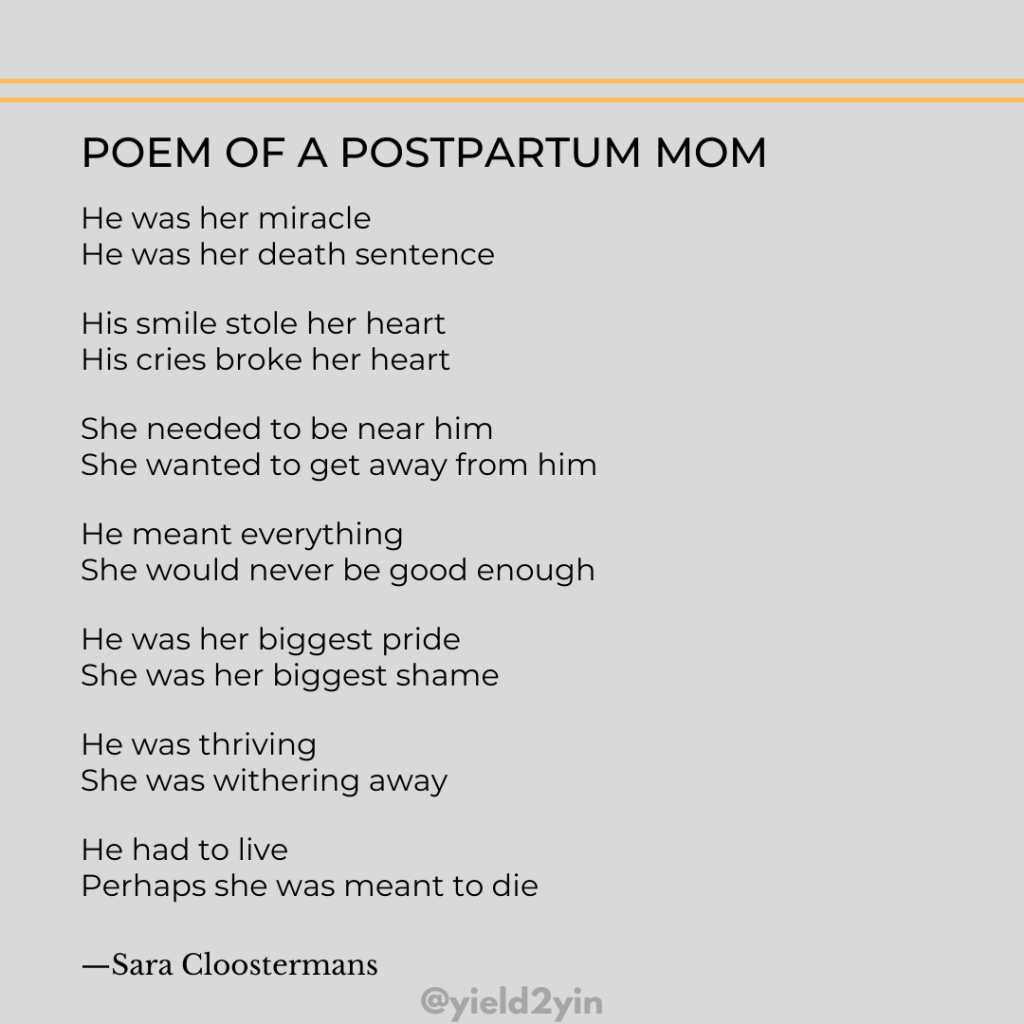
The responsibility of taking care of my tiny newborn was all-consuming and too much to handle. It was beyond “killjoy” because I felt no joy in the first place. His level of fragility and vulnerability seemed unbearable. His dependence on me was too much. I started thinking that T. and I could not co-exist AND both survive (let alone thrive).
I became convinced I was supposed to have died in that hospital because I felt like such a bad mother. It seemed like my colicky baby told me every day how poor of a job I was doing. I firmly believed his level of unhappiness stemmed from me not knowing how to properly attune to his needs and wants. T. was inconsolable. What was wrong with me that I could not accomplish the simple task of comforting my own baby? I felt that T. (and my husband) deserved better.
It was my downstairs neighbor, who happened to be a psychiatrist, who diagnosed me with major depressive disorder when my baby boy was 6 weeks old. And it was my husband who then had the idea to do an internet search on his work computer to see what this was all about.
He was able to pull up two stories of other mothers with similar postpartum symptoms to the ones I was dealing with. He printed them out and brought both copies home.
That was my “There were others!” moment. Other women felt how I had been feeling after having my first baby: miserable and alone. Receiving this crumb of validation was enough to make me feel more “normal” – maybe I had not completely lost my mind after all?
I was still doubtful though because neither one of the mothers mentioned having symptoms of postpartum OCD (Obsessive-Compulsive Disorder), which is what I was experiencing. I knew nothing about the most misunderstood and misdiagnosed of the perinatal disorders according to Postpartum Support International.
Let’s Talk about Peripartum OCD
My “obsessions” – anxious thoughts that are unwanted, persistent, and disturbing in nature – were causing me extreme distress. The anguish I experienced, caused by the many intrusive thoughts of harm happening to my newborn baby in the most horrible ways, consumed every part of my being.
What do these thoughts mean? And what do they say about me? If I can have these types of dark and violent thoughts, does that mean that I could act on them?
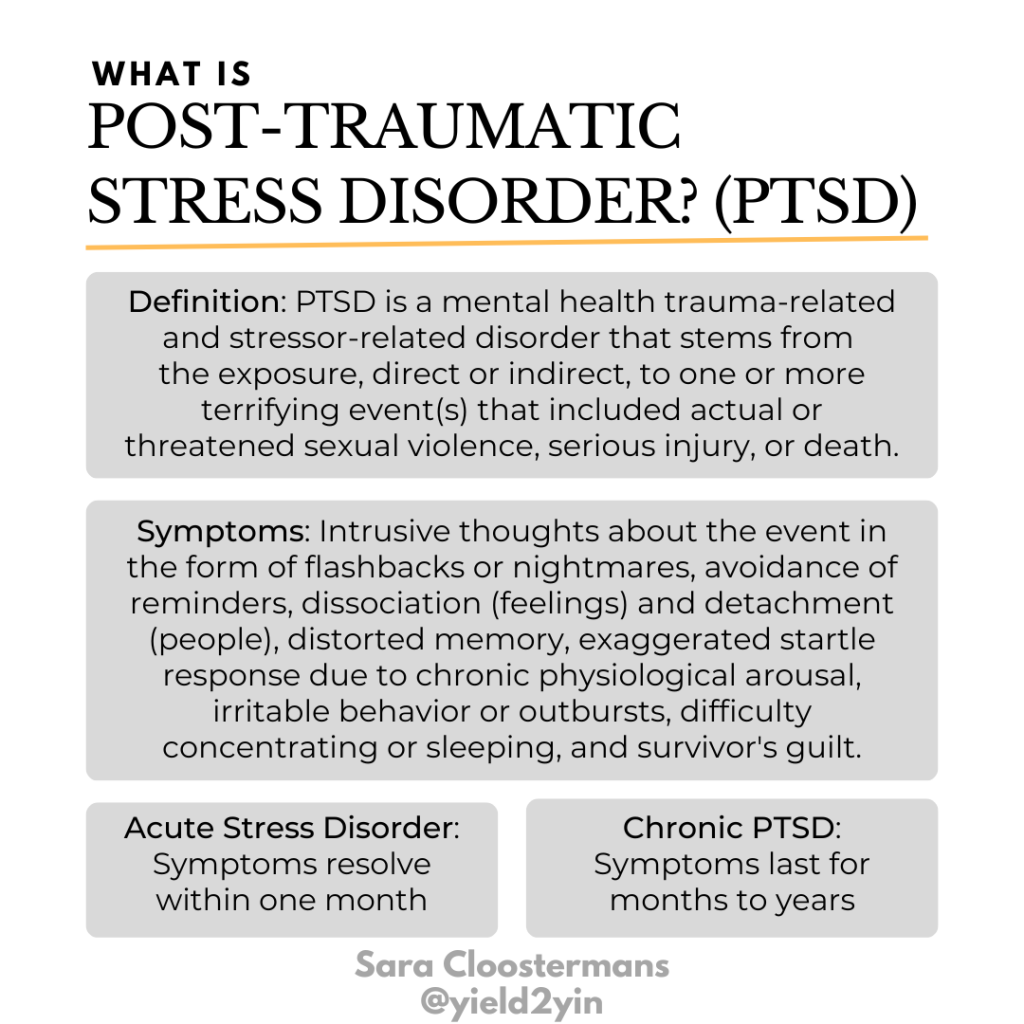
The fear of that happening was truly traumatizing and elicited typical trauma responses throughout my postpartum days and months. The PTSD symptoms I experienced were:
- Intrusive re-experiencing of the childbirth
- Flashbacks and nightmares
- Persistent increased arousal (difficulty sleeping, hypervigilance)
- Anxiety and panic attacks
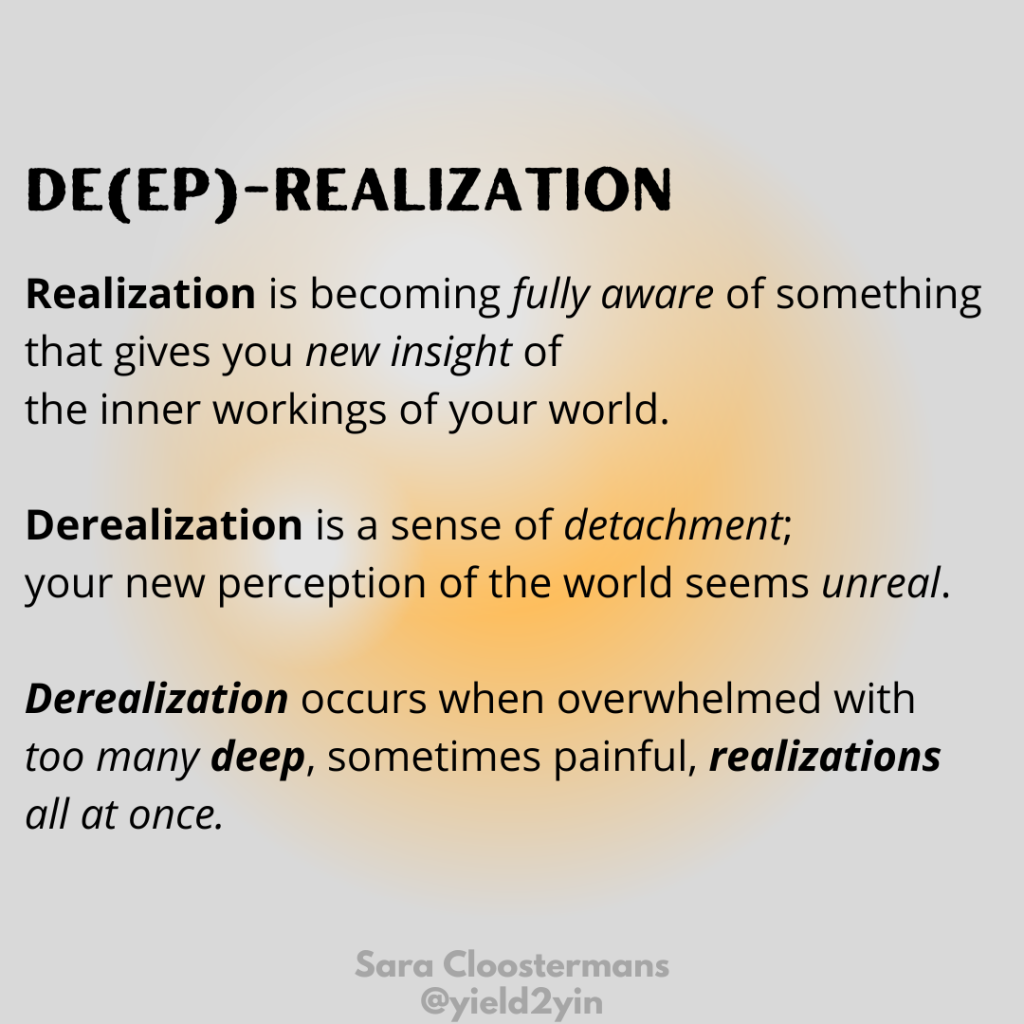
- Derealization
The many painful and scary feelings I experienced were so high in intensity, frequency, and duration that they became debilitating. Summed up, I felt alone and lonely, scared and out-of-control, incapable and worthless, helpless and hopeless, confused and conflicted, guilty and ashamed, …
and potentially dangerous and unsafe.
Have I turned from being a gentle human being all the way up to T.’s birth into a potentially dangerous mother immediately after his birth somehow? Just like that… overnight; is that possible?
I was not sure, and because I did not trust myself to be left alone with my newborn, I asked for someone to be always with me. To this day, I still feel sad sometimes, looking back at my younger self not knowing what was really going on.
If only I had known then what I know now: that typical intrusive thoughts can include irrational fears of contamination, fears of accidentally harming the baby, or thoughts of intentionally hurting the baby. Consequently, mothers may develop compulsions (to alleviate the anxiety), such as excessive cleaning, constantly checking on the baby, or avoiding the baby out of fear of acting on an unwanted violent thought.
If only I had known then what I know now: that anxious thoughts are “ego-dystonic” thoughts – when one is afraid of their own thoughts and knows that their thoughts are wrong and inconsistent with their self-concept, worldview, and moral system vs. aligning with their aggressive, scary thoughts.
If only I had known then what I know now: that I was anxious. I was not psychotic. With postpartum psychosis, which is very rare (0.1- 0.2%), mothers have “ego-syntonic” thoughts – when one believes their bizarre thoughts, which are delusional beliefs, to be true. Keep in mind that delusions are not always destructive in nature, and there is not always a risk of harm to self or the baby, but there can be (suicide = 5%, infanticide = 4% of the 0.1 – 0.2%), so it is imperative that the situation is treated as an emergency and the mom receives help immediately.
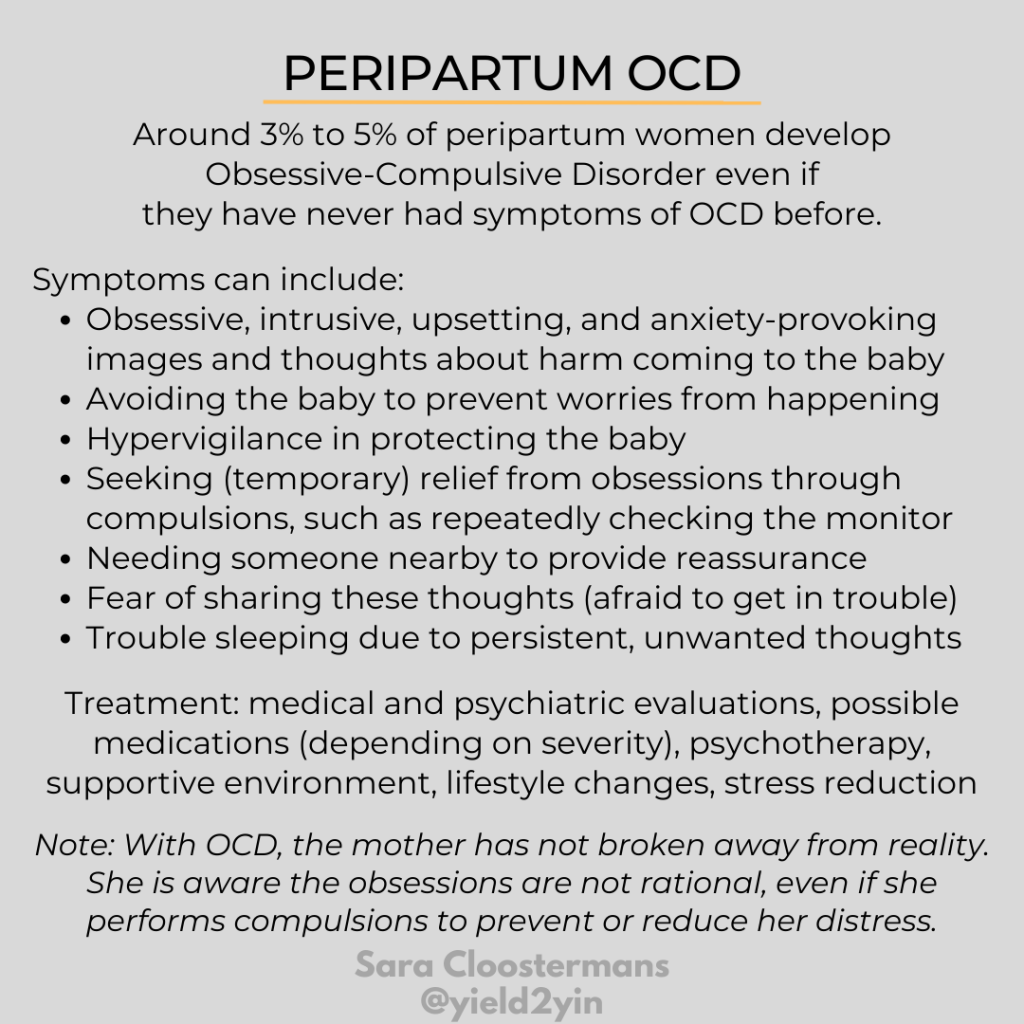
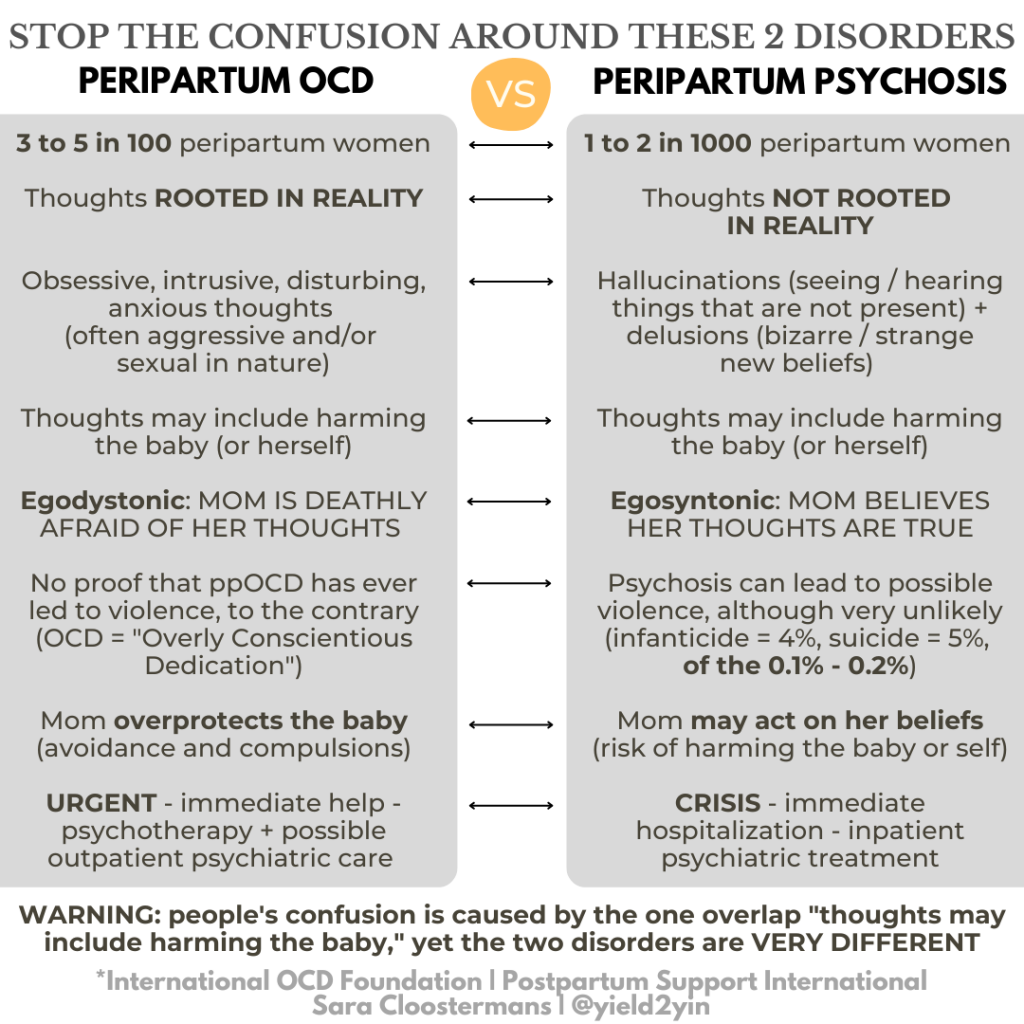
In short, postpartum OCD, which is what I had, and postpartum psychosis are two very different conditions. If you are interested in learning a bit more about the difference between the two mental health diagnoses, read the paragraph “Is pOCD related to postpartum psychosis?” (and now you know that the answer is “no”) on page 2 of the article by Jonathan Abramowitz, Ph.D., ABPP, What are Postpartum and Perinatal OCD? published by the International OCD Foundation.
From “Rock Bottom” to “Back on Top”
I can honestly say that up until 6 weeks postpartum, when I was finally diagnosed with major depressive disorder, I had probably slept no more than 2 hours a night (maybe 3 “on a good night”). And on top of that, due to suppressed appetite and GI issues, I had lost at least 30 lbs. (more than I had gained during my pregnancy).
Once I had my diagnosis, we kicked my treatment into gear. The interventions that helped me the most with making it “back on top” included:
- Medication/Nutrition/Sleep: I was on Elavil, a tricyclic antidepressant, for 6 months. This brand name has been discontinued in the US, but the generic alternative, Amitriptyline, is still approved by the FDA. As far as I know, it’s not ever used to treat PMADs in the US. The day after I began taking this psychotropic medication (sometime during week 7 after T.’s birth) was the day that I started eating again during the day and sleeping again at night.
- Therapy/Calling: I saw a therapist for a few months for individual sessions mostly; my husband joined me for one or two of them. Therapy helped me feel more normal; I was accepted and understood by someone whose opinion I trusted. It was during one of my first therapy sessions that I realized I wanted to become a therapist myself one day.
- Family/Support: With his frequent flier miles, my husband flew out friends and family members until T. was 3 months old and his colic stopped, so for about a month and a half. Being in the company of my loved ones made all the difference. My mother-in-law was especially helpful during this time; I will never forget her kindness and will be forever grateful to her.
- Walking/Exercise: I needed to be out in public and outside. It made me feel less alone and more connected to the world. We lived nearby two different lakes right by our house in Zehlendorf; one is called “Krumme Lanke” (just under an hour walk from where I lived) and the other “Schlachtensee” (just over an hour and a half walk). I walked around either one of these lakes almost every day pushing T.’s “Teutonia” baby carriage. On the way home from the lake, I picked up groceries. At the grocery store, I snapped T. in the front baby carrier and piled all the groceries into his carriage. Walking so many miles a day pushing a heavy stroller, resulted in me being in the best shape I had ever been in (not by choice).
- Friends/Visits: I occasionally tried to visit a friend, but unfortunately most of my friends were working during the day (and none of my friends had children yet). When my husband and I moved to Berlin, we met all our friends through my work. I worked for Berlitz Language School (up until I had T.) and our friends were all language teachers. Even though they came from all over the world, they all knew English. We were a very eclectic (and fun!) international group. Anyways, I managed to visit a friend here or there during their lunch break on Kurfürstendamm (where the language school was located), one of the most famous avenues in Berlin (like Fifth Avenue in NYC); they all loved doting on baby T. whenever they had a chance to see him.
- Sightseeing/Excursions: Several times a week, I would pack up T.’s diaper bag as soon as my husband left for work. I would then leave the house for most of the day because I was afraid of being home alone for long stretches at a time. The U-Bahn (underground railway) took us either into the center or to the outskirts of Berlin, whichever I was feeling that day. Let’s just say I became really familiar with the city and its bordering cities, such as Potsdam with the iconic Sanssouci Palace. Ironically, “sans souci” is the French phrase for “without worry”.
- Playgroup/Socializing: I joined a playgroup that consisted of other American expats living in Berlin; we all took turns hosting. I was much more extroverted then than I am now and being around other people’s energy helped recharge my mental health battery.
- BFF/Mom Friend: I made a close mom friend, Suzanna, from Italy, whom I met at Lamaze class, but of course, her little boy, Guglielmo (Italian for William), born 5 days after T., was “perfect” all the time. Motherhood came so easily to her – she described her fourth trimester as the most “peaceful” time of her life. Needless to say, our experiences could not have been more different.
- My husband/Hope: My husband was the one who gave me a sense of hope when I could no longer see the future; when all I saw and felt was the present moment, which was dreadful and felt permanent. My husband was the one who reminded me that T. was not going to be a small baby forever and that someday, we would buy him his first pair of shoes and T. would learn how to walk. My husband was the one who told me that someday, we would make T. a birthday cake and help him blow out his candle(s), and that eventually, T. would be blowing out his own candles. My husband was the one who would have me listen to Enya songs to help me relax and would serve me warm “calming” tea (although he added Baileys too, which in hindsight, adding an Irish cream liqueur may not have been the best idea, but hey, I felt the love). He was also the one who told me several times a day, for many months, “It will get better, Sara,” which became my go-to mantra. And he ended up being right… it did get better. I would say that by the time T. was about to turn one year old, which is when we moved back to the United States, I felt strong and healthy again (and “sans souci”).
Fast Forward 25 Years

Over time, medication, support (family, friends, therapy, playgroup), and self-care (walking, nature, city trips) were the different treatments that helped me recover and make it “from the depths of despair back to the surface”.
Through my personal journey, I came to a better understanding of mental illness, which helped me find new meaning in life, especially in my career. My postpartum experience led me to a career that I have loved for the past two decades practicing as a therapist specializing in PMADs. While I haven’t gone through every situation my clients have gone through, I know what it’s like to feel alone, confused, desperate, exhausted, miserable, and scared. I can connect with them on a deeper level.
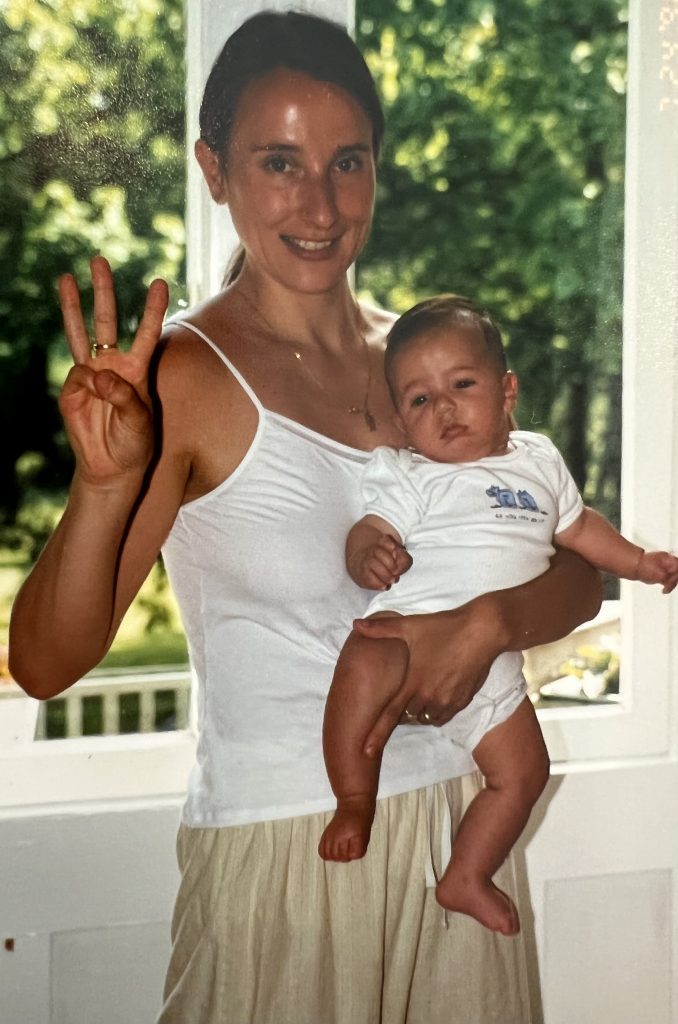
And the kids turned out alright… 🥰
T. is a great kid; closely connected to his loved ones, both family (incl. me 😉) and friends, easy-going and outgoing, smiley and sweet, generous with time and money, and adventurous with food and travel. He just graduated with his law degree and is starting his first “real job” this month as a patent attorney. He will be working remotely from LA where he lives with his long-term girlfriend, who is as sweet as he is, and their 2 big, black cats; 2 brothers, Forrest and Khalil. T. and his girlfriend love living in the biggest entertainment capital of the world and taking advantage of the myriad of activities and attractions Los Angeles has to offer.
My youngest L. lives at home, with my husband and I, in San Diego, and is taking her pre-nursing classes in preparation for applying to a 4-year nursing program, ideally at a local college. L. is the quintessential Southern California girl, born and raised, and is happiest in the water, ocean water or pool water. She’s not picky as long as she can swim or play waterpolo (and watch beautiful sunsets).


When I look at the amount of pressure society puts on new parents to focus on “infant bonding,” I don’t find it helpful. On one hand, we urge them to spend as much time with the baby as they possibly can, especially during the baby’s first year of life, yet on the other hand, we don’t give them the time, nor the resources and support to make that a reality. New parents are often left to their own devices and must return to work within an unreasonable amount of time, especially in the US (unless they are stay-at-home parents, of course).
Being a mom of two grown children, I’ve come to realize that, absolutely, bonding with your baby is important for their brain growth and their future attachment style, but there is time: plenty of time. Even though, ideally, the initial main bond is between the infant and the primary caregiver, it does not have to be. It’s not always possible (as in my case), and that’s OK. If there are other loving caregivers who provide the baby with lots of smiles and eye contact, loving caregivers who talk, read, and sing to the baby, loving caregivers who respond to the baby’s cries with cuddles, and so on, the chances that our kiddos are going to be fine are pretty darn high. Bonding with mom does not have to be instant. You have a lifetime of opportunity to show your children that they mean the world to you.
Just recently T. told me, “You know, mom, I’m now close to the age that you were when I met you.” He was referring to his current age (25) and my age when I had him (27), and his earliest childhood memories as a toddler. T. continues, “I still feel like a kid inside, so you must have felt like you were still a kid when you had me.”
Well put, T.; I could not have said it better. An adult kid who needed mothering. The “Mother” archetype represents qualities such as “love, nurturing, and protection.” That is what I needed. That is what we all need when we become new parents.
Change starts with awareness. Only once we educate ourselves can we put ourselves in a position to make informed decisions and to take effective action steps to help ourselves and others. Instead of setting new families up to fail, we can then create a compassionate culture that sets our families up to succeed.
Well-supported parents are much better equipped to provide improved and increased self-care, and then fully be there for their babies and other family members.
Mothering the mother will lead to healthier and happier families, communities, and societies.
If Any of This Feels Familiar to You and You Need Help…
- Reach out for support – from family, friends, your doctor, and/or a therapist (preferably one who specializes in PMADs)
- Educate yourself (and ask those closest to you to do the same). Here is a great list of resources to get you started:
- Realize how normal you are – take a deep breath of reassurance. You are not alone. Local moms’ groups can be a great place to connect with others who are going through / have gone through the same thing!
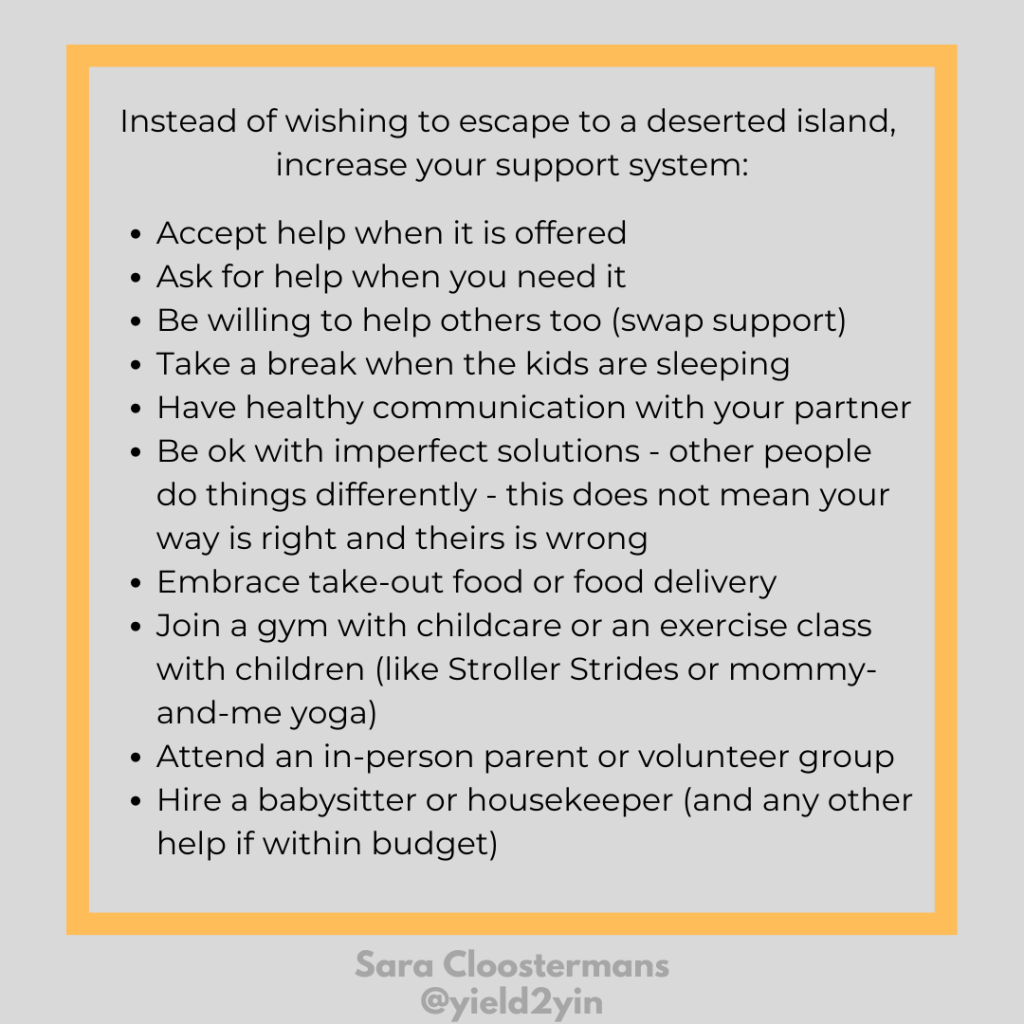
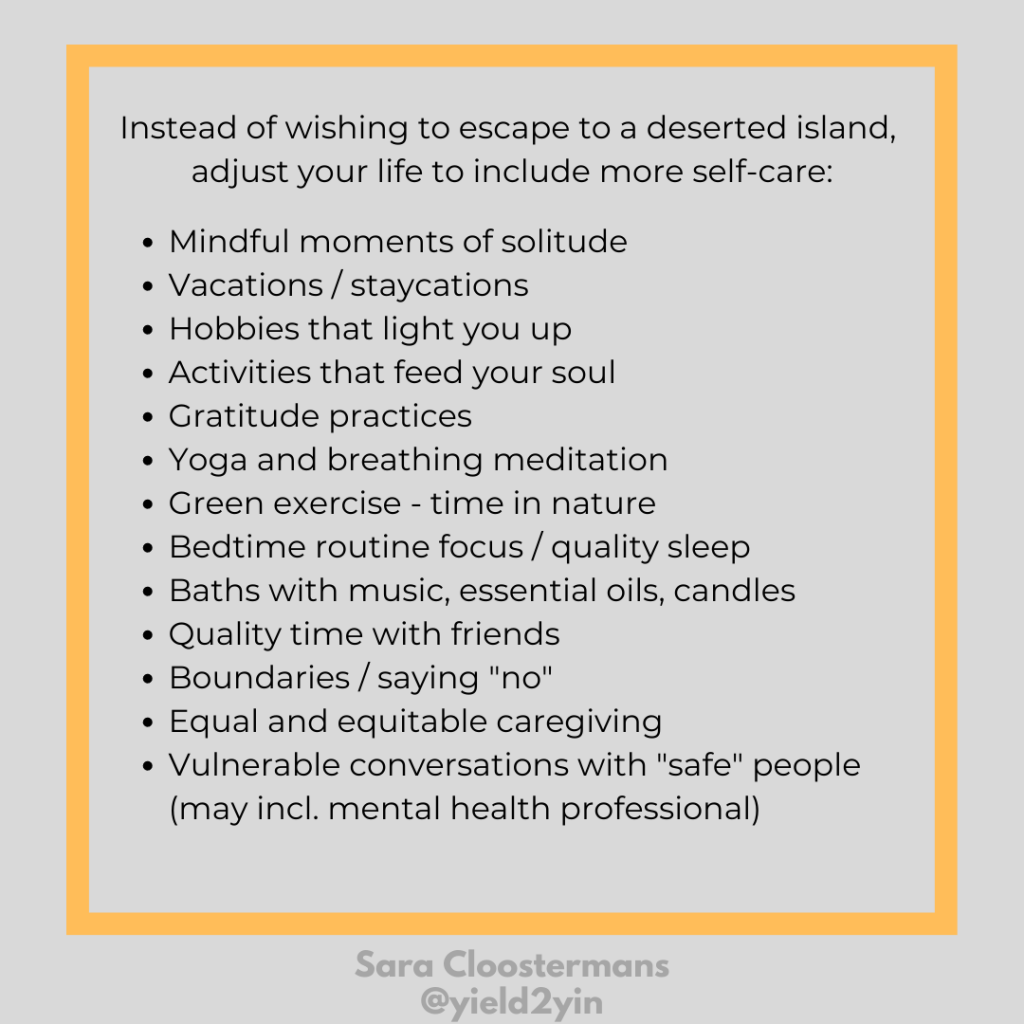
Side note: If you find yourself wishing to “escape” and lead a pre-parent and childfree life again, here are some softer suggestions that are probably more in tune with what you (and your family) really need and want:
If Someone You Know Needs Help…
If somebody you care about is in their postpartum period, here are a few helpful tips:
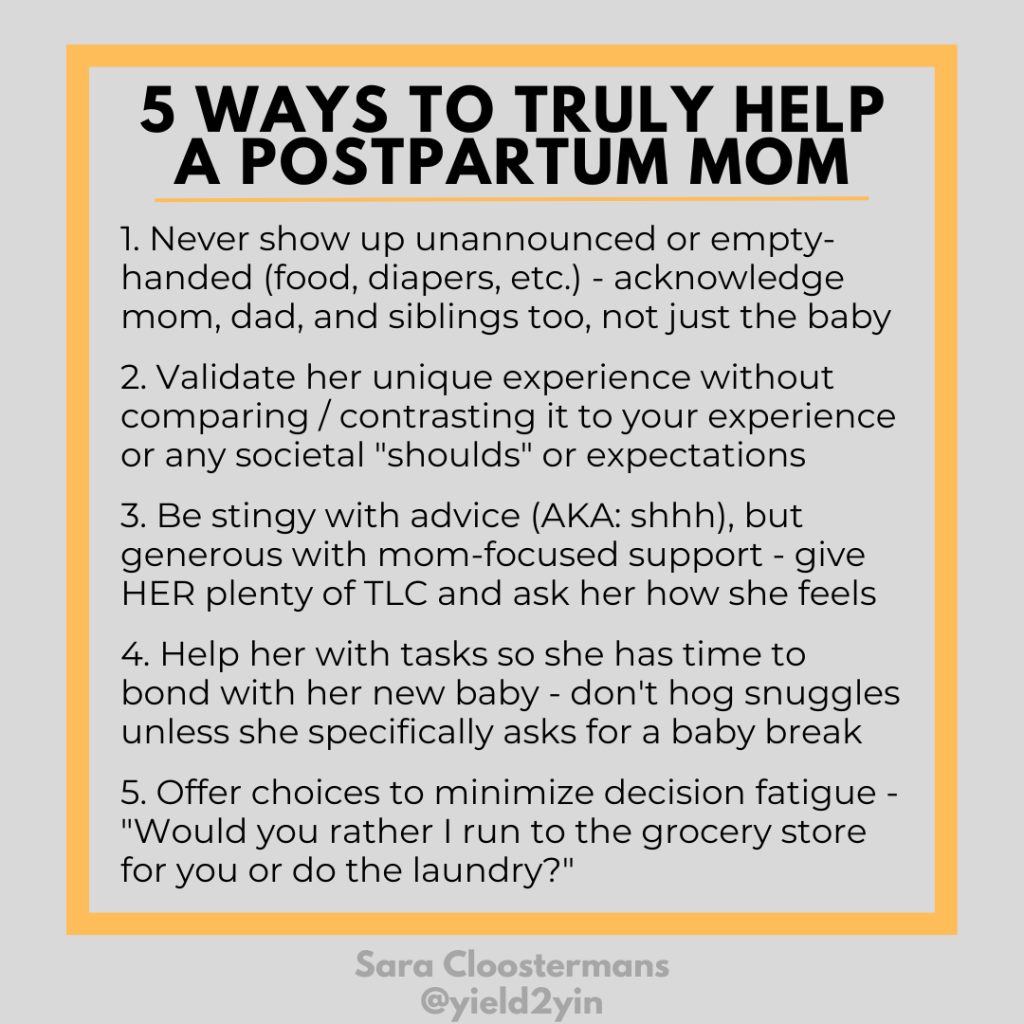
The October blog, “Tips to Help New Moms and Their Families throughout Pregnancy and Postpartum” will be even more helpful! (be sure to sign up to get the monthly blogs delivered straight to your inbox if you don’t want to miss it!)
Resources
- Postpartum Health Alliance
- Postpartum Support International
- Perinatal Mental Health Alliance for People of Color
- The Shades of Blue Project Maternal & Mental Health Resource Center for Black and Brown Birthing People
- The Postpartum Stress Center
- The Center for Women’s Mental Health at Mass General
- The Motherhood Center of New York
- Maternal Mental Health Alliance UK
Related Posts
- Hard Work Is Relative, So Be Compassionate
- We Cannot Have It All
- Don’t Forget Change Requires Change
Yield2Yin
- Healing Card Deck: A Therapist’s Advice 55-Card Healing Deck by Sara Cloostermans
- Spark Mamas: Meaningful Gift Ideas to Help Mothers Thrive through Parenthood
- Book Recommendation: Good Moms Have Scary Thoughts: A Healing Guide to the Secret Fears of New Mothers by Karen Kleiman (Author), Molly McIntyre (Illustrator)
- Mantra: I AM VULNERABILITY // with diaphragmatic breathing
- Yin Yoga Asana: Butterfly Pose