Not very long ago, the way women felt in their minds and bodies during and after pregnancy was entirely hush-hush – considered private, and at times even shameful. Many women were drowning, and nobody was paying attention.
Luckily, the tides are changing, and our culture is warming up to the idea that talking about postpartum health – especially postpartum mental health – is essential for healthy moms, healthy babies, and a healthy society.
Yet many of us aren’t well-versed in the various ways a mixture of hormones and experience (past trauma, recent loss, bad marriage/partnership, lack of social support, incl. return-to-work support, etc.) can shape a woman’s mental health during pregnancy and postpartum.
So, consider this article your guide to Postpartum Mental Health 101.
It’s a must-read for anyone who may become pregnant, is pregnant, is postpartum, was postpartum… and for anyone who knows a woman who falls under any of these categories. In short: everyone can benefit from this info!
“Postpartum” or “Peripartum”?
Most of the time, the word “Postpartum” refers to mental illness that begins AFTER DELIVERY of the baby. However, due to hormonal changes, and adverse past or current circumstances, pregnant women can begin experiencing mental health symptoms DURING PREGNANCY.
A broader term encompassing both the postpartum period AND the pregnancy is therefore more accurate: “Peripartum” (or “Perinatal”).
When Can You Experience Peripartum Mental Health Illnesses?
Every woman’s experience is different. Typically, if any of these disorders show up during pregnancy or within the first 12 months after delivery, they are considered “Peripartum” or “Perinatal”. They are now commonly referred to as “PMADs” – Perinatal Mood and Anxiety Disorders.
Some women experience a PMAD during their pregnancy, and others within the first couple of weeks or months after delivery. Still others don’t begin to display symptoms until after their babies are already walking. For some women, the sudden hormonal shifts of weaning can also trigger a type of PMAD.
What Are the Seven Types of Perinatal Mood and Anxiety Disorders (PMADs)?
- Baby Blues
- Peripartum Depression
- Peripartum Anxiety
- Peripartum Obsessive Compulsive Disorder
- Peripartum Bipolar Disorder
- Peripartum Post-Traumatic Stress Disorder
- Peripartum Psychosis
Note: in the DSM-V these disorders are not all classified as either a “mood” or an “anxiety” disorder (or not recognized at all as with the baby blues); yet, for the purpose of simplification, all 7 disorders are listed under the same title.
1. Baby Blues
The baby blues is a short-lasting condition (1 – 2 weeks) that around 70% to 80% of mothers experience. It does not interfere with daily activities and does not require medical attention.
Symptoms can include:
- Sudden mood changes
- Sadness and tearfulness (for no apparent reason)
- Anxiety and restlessness
- Insomnia (even when the baby is sleeping)
- Fatigue
- Irritability and impatience
- Poor concentration
Treatment: typically, no treatment is required since the symptoms are mild and transient
2. Peripartum Depression
During pregnancy and/or up to 12 months after birth, 15% to 20% of mothers experience this serious, yet treatable mental health disorder (about 8% to 10% of fathers experience this in the first year too).
“Fifty percent of ‘postpartum’ major depressive episodes actually begin prior to delivery. Thus, these episodes are referred to collectively as peripartum episodes. Women with peripartum major depressive episodes often have severe anxiety and even panic attacks.” (PSI)
Symptoms can include:
- Feeling sad and crying for “no reason”
- Feeling angry or irritable
- Feeling hopeless, worthless, or guilty (for being a “bad” or an “ungrateful” mom)
- Changes in appetite (lack of or increased)
- Insomnia (trouble falling and/or staying asleep) or hypersomnia (sleeping too much)
- Difficulty concentrating and making decisions
- Loss of energy for / interest and pleasure in activities once enjoyed
- Lack of interest in the baby / not feeling bonded
- Fear of harming the baby and/or oneself
- Thoughts of death or suicide
Screening tool: The Edinburgh Postnatal Depression Scale (EPDS)
Treatment:
- Medical evaluation to rule out physical problems (thyroid issues, vitamin deficiencies)
- Psychotherapy, e.g., CBT (Cognitive Behavioral Therapy)
- Psychiatric evaluation and possible psychotropic medication(s) – depending on severity
- Supportive environment (family, friends, moms support group)
- Lifestyle changes (improved nutrition, exercise, sleep hygiene)
- Stress reduction (relaxation training, yoga, meditation, journaling, massage, etc.)
Hot off the press:
On August 4th, 2023, the FDA approved ZURZUVAE (zuranolone), the first and only oral medication shown to be effective in treating women with postpartum depression expressly.
- FDA – FDA Approves First Oral Treatment for Postpartum Depression
- PBS – The FDA approves the first pill specifically intended to treat postpartum depression
- CNN – FDA approves first postpartum depression pill in the US
3. Peripartum Anxiety
Around 6% to 16% of women experience an anxiety disorder during pregnancy, 10% to 17% during the postpartum period, and 2/3 of women with peripartum depression also have an anxiety disorder.
Symptoms can include:
- Feeling panicky for no good reason
- Inability to sit still or relax
- Feeling on edge and irritable
- Physical symptoms (dizziness, hot flashes, nausea, rapid heart rate, etc.)
- Racing thoughts / sense of impending doom
- Excessive worrying / obsessing over irrational fears
- Blaming oneself when things go wrong
- Changes in appetite (lack of or increased)
- Insomnia (trouble falling and/or staying asleep)
Screening tools: Matthey Generic Mood Question or EPDS Anxiety Subscale
Treatment:
- Medical evaluation to rule out physical problems (thyroid issues, vitamin deficiencies)
- Psychotherapy, e.g., CBT (Cognitive Behavioral Therapy)
- Psychiatric evaluation and possible psychotropic medication(s) – depending on severity
- Supportive environment (family, friends, moms support group)
- Lifestyle changes (improved nutrition, exercise, sleep hygiene)
- Stress reduction (relaxation training, yoga, meditation, journaling, massage, etc.)
4. Peripartum Obsessive Compulsive Disorder (ppOCD)
Around 3% to 5% of peripartum women develop ppOCD symptoms even if they have never experienced symptoms of OCD before. Women who already had or have OCD are more likely to have exacerbated ppOCD symptoms during the peripartum period.
Symptoms can include:
- Obsessive, intrusive, upsetting, and anxiety-provoking images and thoughts, e.g., about harm coming to the baby
- Avoiding the baby to prevent obsessive worries from coming true
- Seeking (temporary) relief from obsessions through compulsions, such as repeatedly checking the baby monitor, Googling the same question over and over again, or excessively washing hands
- Needing someone to always be with you, either in-person or on the phone, to provide reassurance that your obsessive, intrusive thoughts are not going to come true
- Trouble sleeping due to persistent, unwanted thoughts
- Fear of sharing these obsessions and compulsions with a trusted friend or therapist, afraid you may get in trouble for having such disturbing or violent thoughts
- Hypervigilance in protecting the baby
Treatment:
- Medical evaluation to rule out physical problems (thyroid issues, vitamin deficiencies)
- Psychotherapy, e.g., CBT and ERP (Exposure and Response Prevention therapy)
- Psychiatric evaluation and possible psychotropic medication(s) – depending on severity
- Supportive environment (family, friends, moms support group)
- Lifestyle changes (improved nutrition, exercise, sleep hygiene)
- Stress reduction (relaxation training, yoga, meditation, journaling, massage, etc.)
Note: OCD used to be classified under anxiety disorders, but in the 2013 DSM-V edition OCD was reclassified under a new disorder class, Obsessive-Compulsive and Related Disorders, with the addition of 2 new specifiers (insight and tic related). Even though there has been this shift, I still tell my clients that ppOCD is an anxiety-related disorder (as well as OC-related), and explain what this added piece of psychoeducational information is based on.
With ppOCD, the intrusive images and thoughts are rooted in anxiety, NOT in delusion. The images and thoughts are NOT acted upon; the mother has NOT broken away from reality. She is fully aware that the obsessions are not rational, even if she performs compulsions to reduce or prevent her distress. Mothers with ppOCD do everything in their power to protect their baby from harm or danger.
5. Peripartum Bipolar Disorder
Bipolar disorder includes two phases – the “high” manic phase and the “low” depression phase – as well as “mixed” episodes when the highs and lows happen at the same time. Risk factors include a previous “manic-depression” and/or family history of bipolar mood disorder.
Symptoms of mania and depression can include:
- Elevated mood and exaggerated confidence
- High energy, racing thoughts, and rapid speech
- Poor judgment and impulsive decisions
- Irritability
- Severe depression
- Little to no sleep
- Trouble concentrating
- Delusions – usually grandiose, but can be paranoid – (in the most severe cases)
- Hallucinations – seeing or hearing things that are not present – (in the most severe cases)
Treatment:
- Medical and psychiatric evaluations, and medications
- Possible hospitalization (in the most severe cases – hallucinations and delusions)
- Psychotherapy, e.g., (MB)CBT (Mindfulness-Based Cognitive Therapy)
- Supportive environment (family, friends, moms support group)
- Lifestyle changes (improved nutrition, exercise, sleep hygiene)
- Stress reduction (relaxation training, yoga, meditation, journaling, massage, etc.)
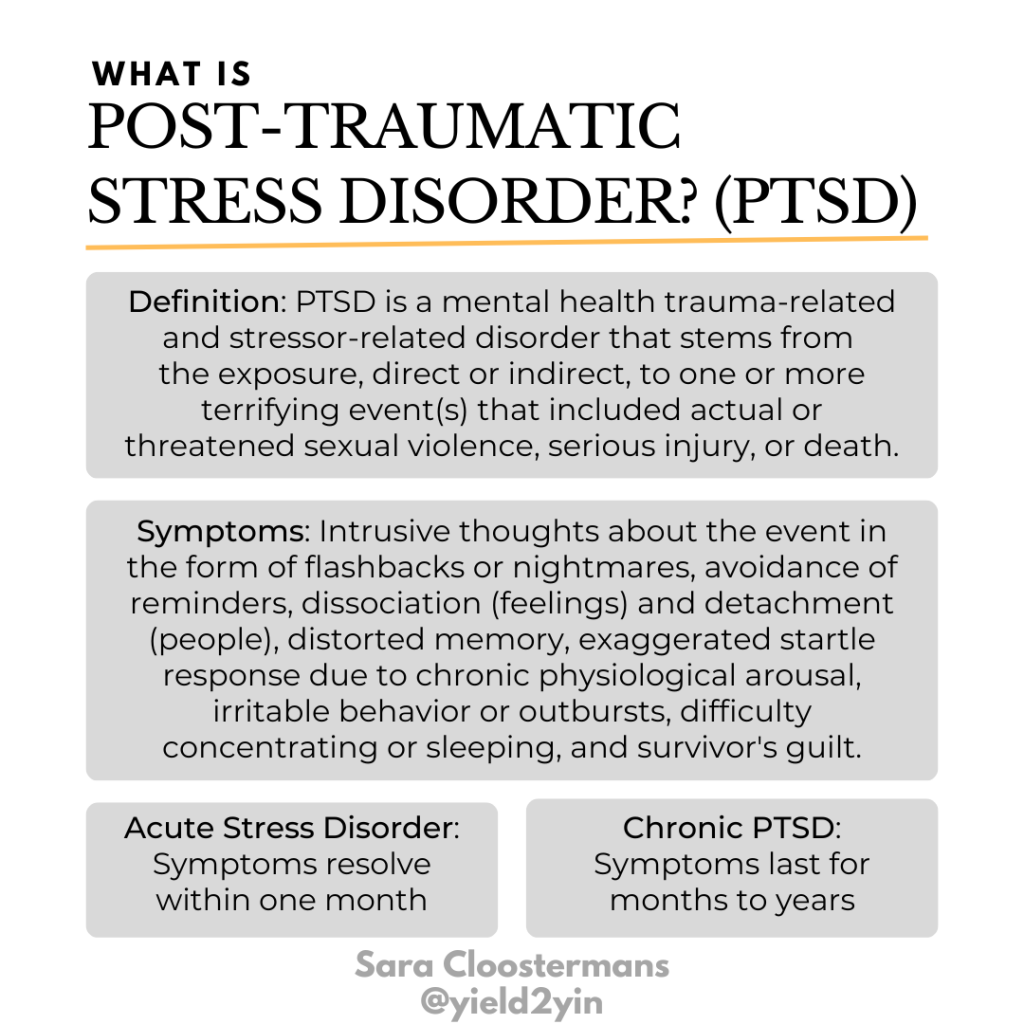
6. Peripartum Post-Traumatic Stress Disorder (ppPTSD)
Around 9% of mothers experience post-traumatic stress disorder due to either a harmful or life-threatening trauma during pregnancy, delivery, or postpartum (a postpartum hemorrhage or a NICU stay, for example).
Symptoms can include:
- Replaying the traumatizing event
- Nightmares or daytime flashbacks
- Avoiding anything that is associated with the traumatic event (like driving past the hospital)
- Feeling irritable or hypervigilant
- Insomnia due to increased physiological arousal caused by sympathetic nervous system activation
- Anxiety and panic attacks
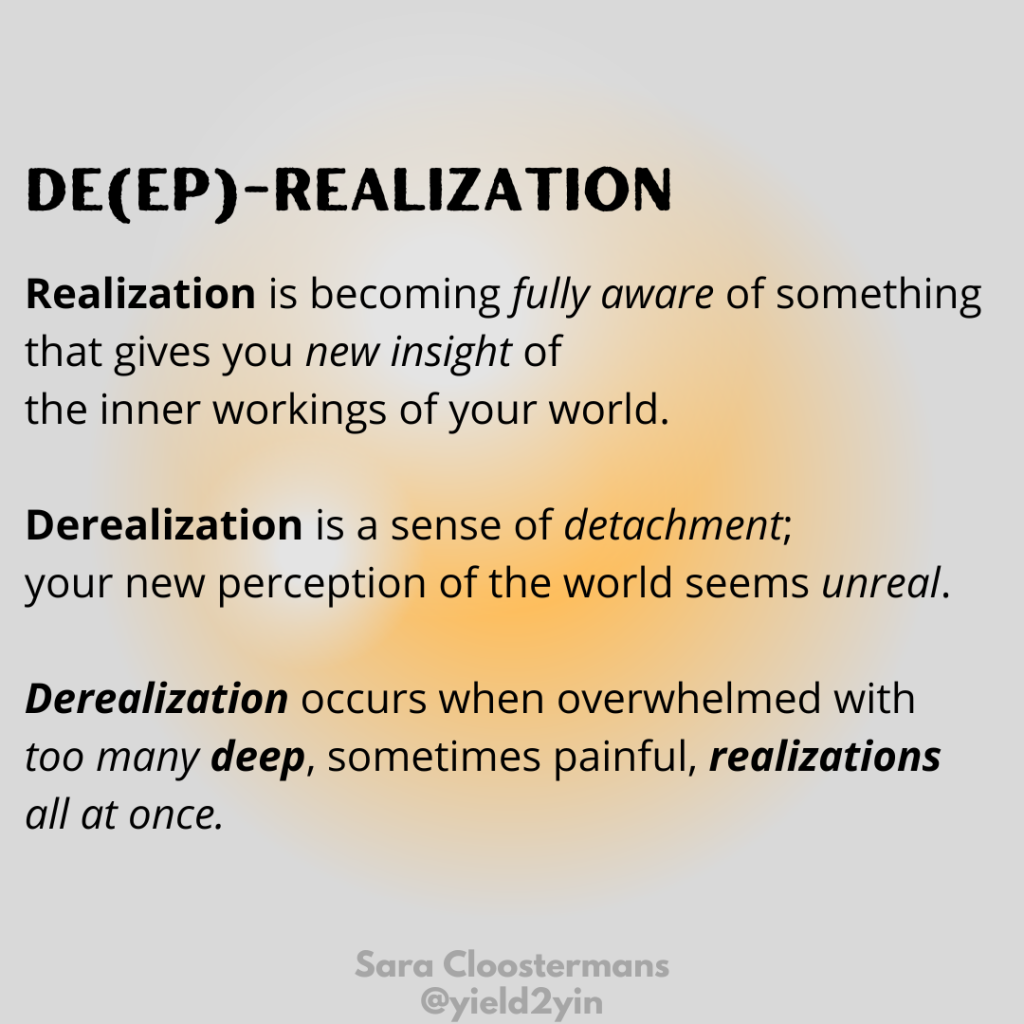
- Derealization (sense of unreality and detachment)
Treatment:
- Medical evaluation to rule out physical problems (thyroid issues, vitamin deficiencies)
- Psychotherapy, e.g., CBT, EMDR (Eye Movement Desensitization and Reprocessing), or Exposure Therapy
- Psychiatric evaluation and possible psychotropic medication(s) – depending on severity
- Supportive environment (family, friends, moms support group)
- Lifestyle changes (improved nutrition, exercise, sleep hygiene)
- Stress reduction (relaxation training, yoga, meditation, journaling, massage, etc.)
7. Peripartum Psychosis
Peripartum psychosis is a condition where a new mother has lost touch with reality. A rare (1 or 2 in 1,000), but serious condition requiring immediate attention. Considered a medical emergency. Risk factors include a personal or family history of bipolar disorder and/or a previous experience with psychosis.
Symptoms can include:
- Severe confusion
- Excessive energy
- Agitation or irritability
- Rapid mood swings
- Delusions (bizarre or strange new beliefs)
- Extreme paranoia and suspiciousness
- Visual or auditory hallucinations (seeing things or hearing voices that are not there)
- Insomnia (trouble falling and/or staying asleep)
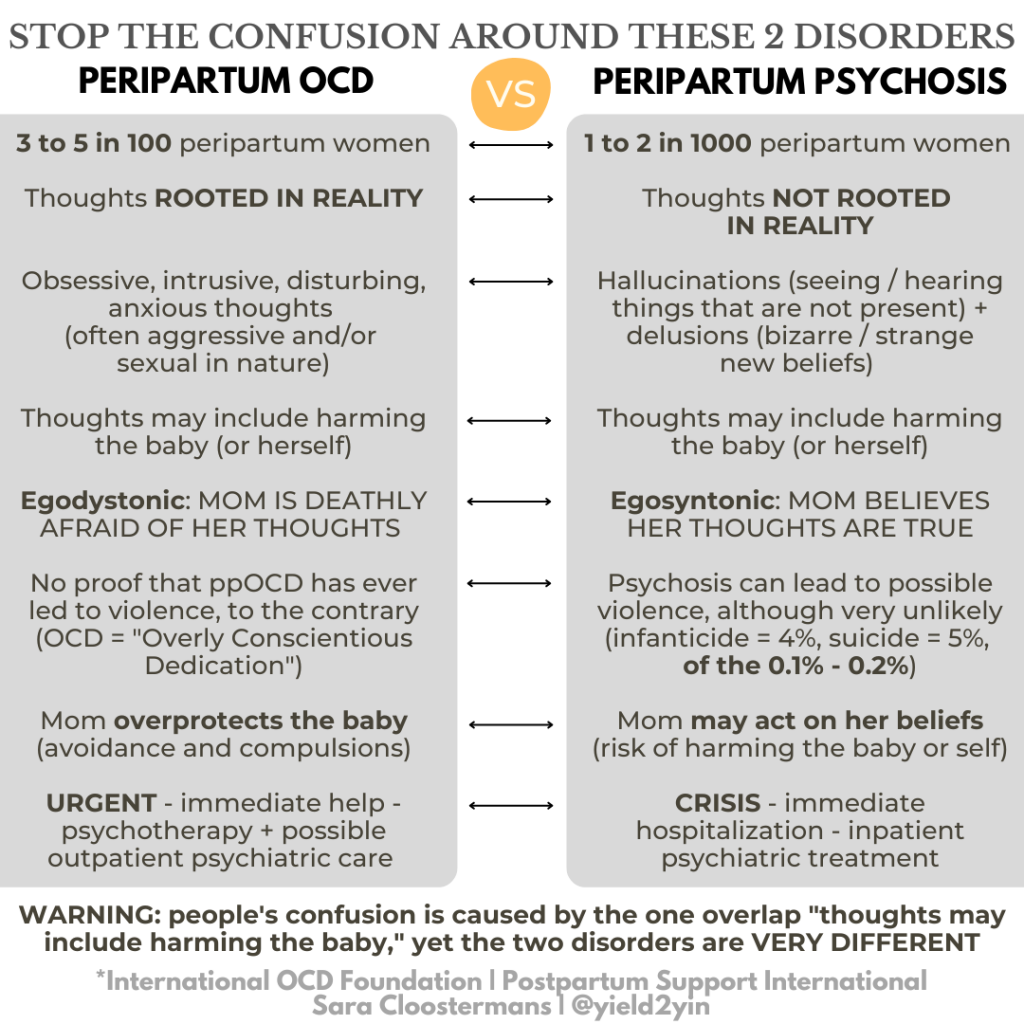
Treatment:
- Inpatient hospitalization – medical and psychiatric evaluations, and medications; if treatment resistant, ECT (Electroconvulsive Therapy)
- Psychotherapy once the mother is stabilized – intensive outpatient therapy, e.g., CBT or Interpersonal Psychotherapy
- Supportive environment (family, friends, moms support group)
- Lifestyle changes (improved nutrition, exercise, sleep hygiene)
- Stress reduction (relaxation training, yoga, meditation, journaling, massage, etc.)
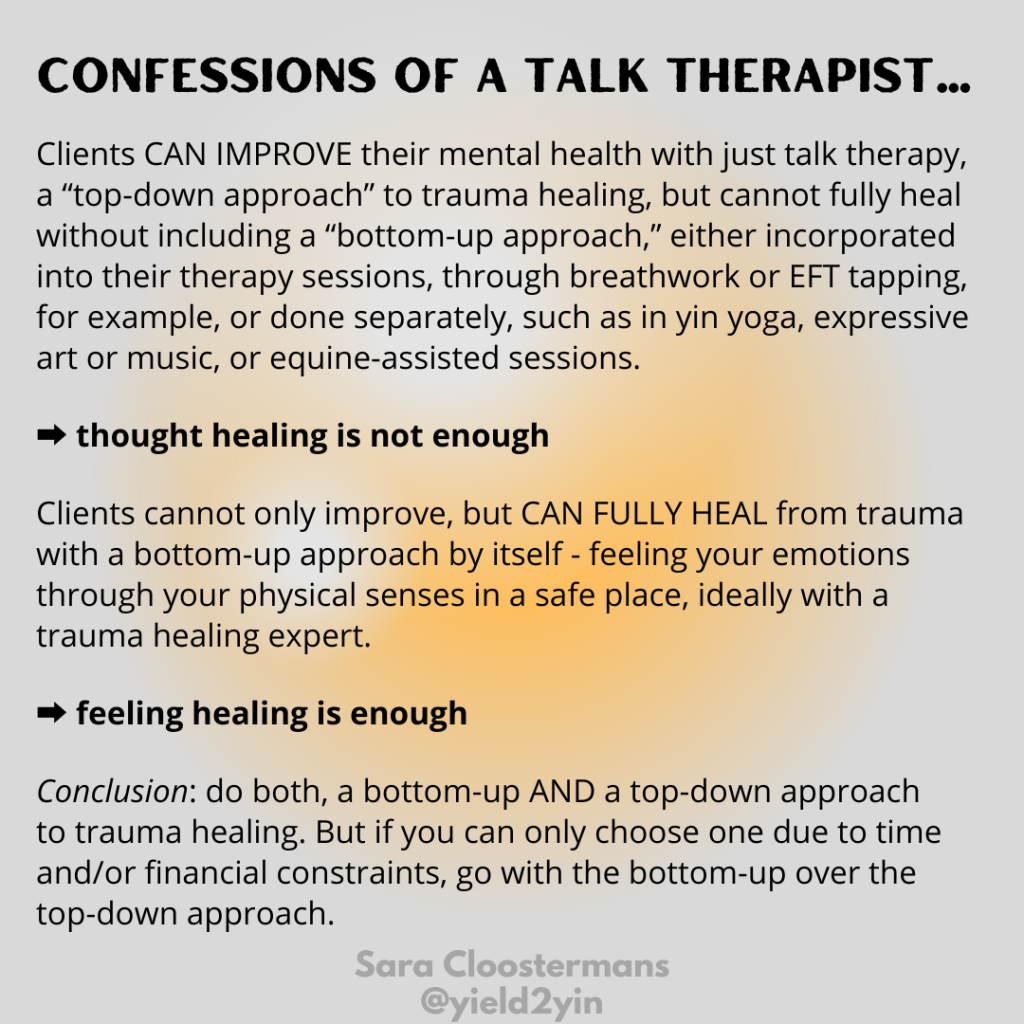
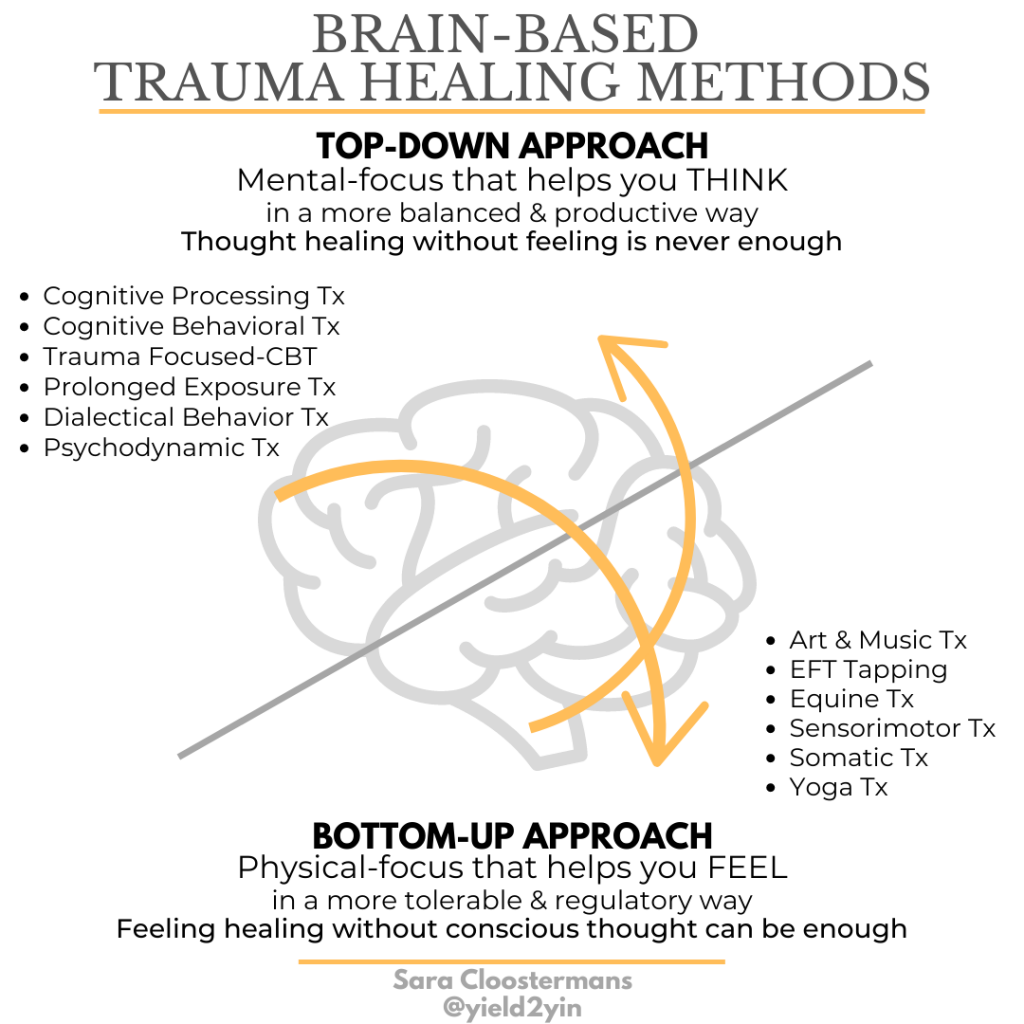
PMADs Treatment Approach: Top-Down, Bottom-Up, or Both?
What Postpartum Mental Health Info Is Still Missing in the DSM-V?
It’s important to understand that our society being behind in validating and diagnosing peripartum mental health disorders means even the Diagnostic and Statistical Manual of Mental Disorders (DSM) is still missing some information. This includes:
- the broader time of onset for symptoms (specifier is currently still only “within 4 WEEKS following delivery” instead of within 12, or even better, 18 MONTHS); fortunately, “with peripartum onset” was finally included in the 5th edition
- the peripartum onset specifier for:
- anxiety disorders
- obsessive disorders
- hypomania
- the importance of diagnostic and statistical criteria through specifiers for:
- anxiety
- mixed anxiety/depressive disorder
- obsessive disorder
- hypomania
- traumatic stress disorders
This information should hopefully become more robust in the coming years as our culture moves even more toward helping pregnant and postpartum women with their mental health and… as more women speak up about their experiences. I will be sharing my personal postpartum experience from 25 years ago in next month’s blog:
“My Postpartum Experience: How I Survived Postpartum Depression and Anxiety”
References
- American Psychiatric Association (APA)
- Diagnostic and Statistical Manual of Mental Disorders, 5th Edition (DSM-V)
- International OCD Foundation (IOCDF)
- Postpartum Support International (PSI)
Resources
- Postpartum Health Alliance
- Postpartum Support International
- Perinatal Mental Health Alliance for People of Color
- The Shades of Blue Project Maternal & Mental Health Resource Center for Black and Brown Birthing People
- The Postpartum Stress Center
- The Center for Women’s Mental Health at Mass General
- The Motherhood Center of New York
- Maternal Mental Health Alliance UK
Yield2Yin
- Healing Card Deck: A Therapist’s Advice 55-Card Healing Deck by Sara Cloostermans
- Spark Mamas: Meaningful Gift Ideas to Help Mothers Thrive through Parenthood
- Book Recommendation: The Postpartum Depression Journal: Prompts and Exercises for Reflection, Healing, and Self-Care by Rachel Rabinor, LCSW, PMH-C
- Mantra: I AM CREATION // repeat with diaphragmatic breathing
- Yin Yoga Asana: Happy Baby Pose